
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Pathophysiology
- Attention to Innate Circadian Rhythm and the Impact of Its Disruption on Diabetes
- Da Young Lee, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Nan Hee Kim
- Diabetes Metab J. 2024;48(1):37-52. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0193
- 2,164 View
- 219 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
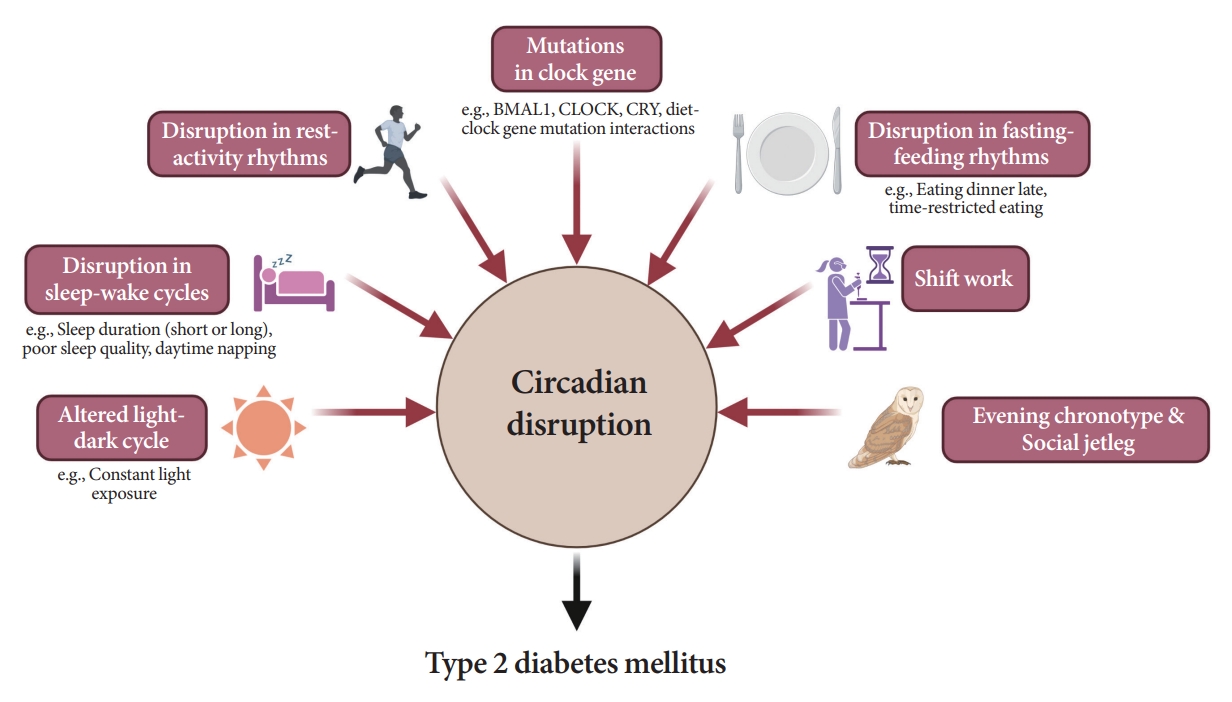
ePub - Novel strategies are required to reduce the risk of developing diabetes and/or clinical outcomes and complications of diabetes. In this regard, the role of the circadian system may be a potential candidate for the prevention of diabetes. We reviewed evidence from animal, clinical, and epidemiological studies linking the circadian system to various aspects of the pathophysiology and clinical outcomes of diabetes. The circadian clock governs genetic, metabolic, hormonal, and behavioral signals in anticipation of cyclic 24-hour events through interactions between a “central clock” in the suprachiasmatic nucleus and “peripheral clocks” in the whole body. Currently, circadian rhythmicity in humans can be subjectively or objectively assessed by measuring melatonin and glucocorticoid levels, core body temperature, peripheral blood, oral mucosa, hair follicles, rest-activity cycles, sleep diaries, and circadian chronotypes. In this review, we summarized various circadian misalignments, such as altered light-dark, sleep-wake, rest-activity, fasting-feeding, shift work, evening chronotype, and social jetlag, as well as mutations in clock genes that could contribute to the development of diabetes and poor glycemic status in patients with diabetes. Targeting critical components of the circadian system could deliver potential candidates for the treatment and prevention of type 2 diabetes mellitus in the future.
- Guideline/Fact Sheet
- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
- Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae Jin Kim, Hyun Min Kim, Jung Hae Ko, Nam Hoon Kim, Chong Hwa Kim, Jeeyun Ahn, Tae Jung Oh, Soo-Kyung Kim, Jaehyun Kim, Eugene Han, Sang-Man Jin, Won Suk Choi, Min Kyong Moon, Committee of Clinical Practice Guidelines, Korean Diabetes Association
- Diabetes Metab J. 2023;47(5):575-594. Published online September 26, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0282
- 5,027 View
- 629 Download
- 7 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
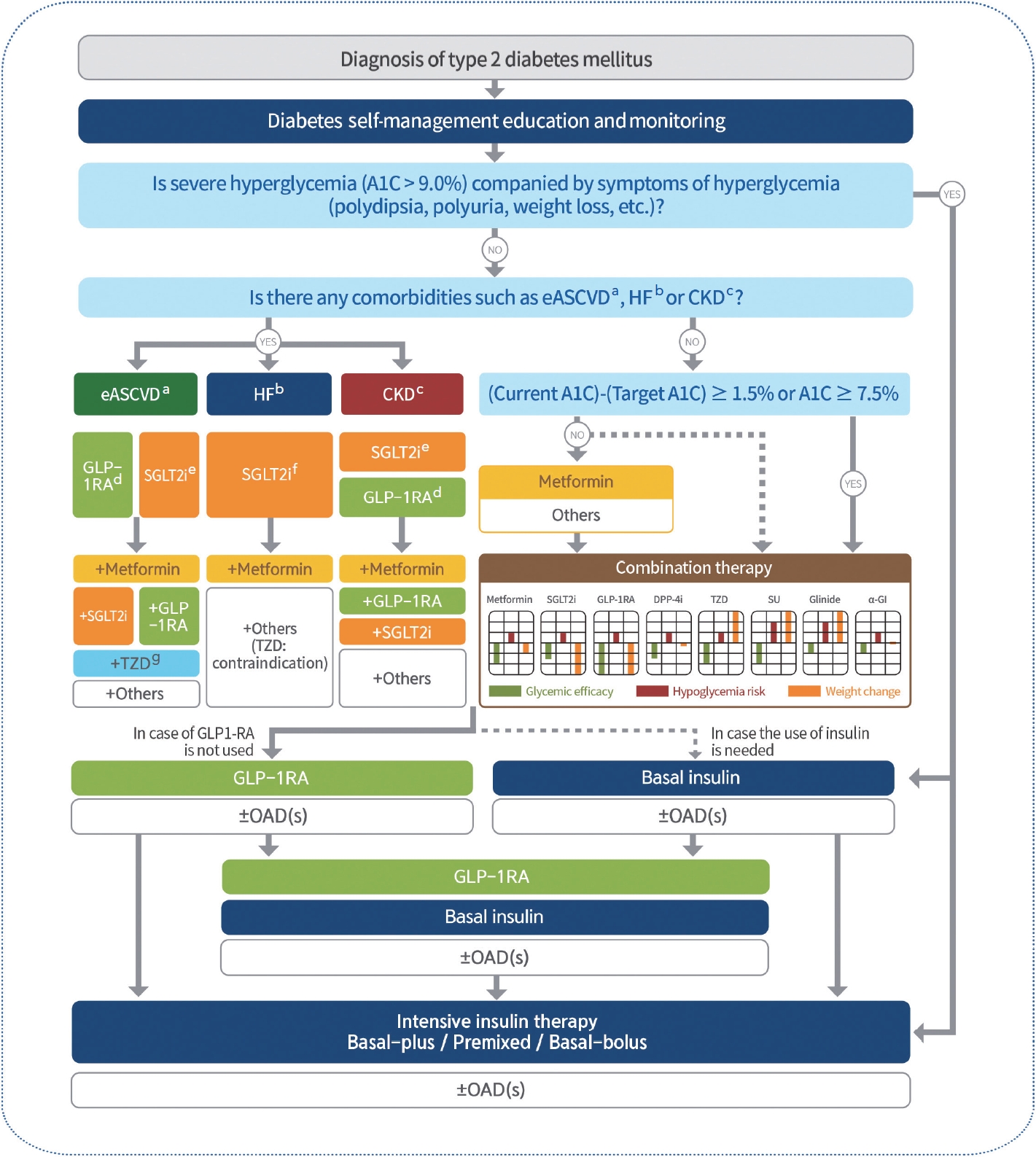
ePub - In May 2023, the Committee of Clinical Practice Guidelines of the Korean Diabetes Association published the revised clinical practice guidelines for Korean adults with diabetes and prediabetes. We incorporated the latest clinical research findings through a comprehensive systematic literature review and applied them in a manner suitable for the Korean population. These guidelines are designed for all healthcare providers nationwide, including physicians, diabetes experts, and certified diabetes educators who manage patients with diabetes or individuals at risk of developing diabetes. Based on recent changes in international guidelines and the results of a Korean epidemiological study, the recommended age for diabetes screening has been lowered. In collaboration with the relevant Korean medical societies, recently revised guidelines for managing hypertension and dyslipidemia in patients with diabetes have been incorporated into this guideline. An abridgment containing practical information on patient education and systematic management in the clinic was published separately.
-
Citations
Citations to this article as recorded by- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Letter by In-Kyung Jeong Regarding Article, Trends in Prevalence of Hypertriglyceridemia and Related Factors in Korean Adults: A Serial Cross-Sectional Study
In-Kyung Jeong
Journal of Lipid and Atherosclerosis.2024; 13(1): 80. CrossRef - Association between cardiovascular disease risk and incident type 2 diabetes mellitus in individuals with prediabetes: A retrospective cohort study
Myung Jin Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee
Diabetes Research and Clinical Practice.2024; 208: 111125. CrossRef - Korea Hypertension Fact Sheet 2023: analysis of nationwide population-based data with a particular focus on hypertension in special populations
Hyeon Chang Kim, Hokyou Lee, Hyeok-Hee Lee, Dasom Son, Minsung Cho, Sojung Shin, Yeeun Seo, Eun-Jin kim, Song Vogue Ahn, Sun Ha Jee, Sungha Park, Hae-Young Lee, Min Ho Shin, Sang-Hyun Ihm, Seung Won Lee, Jong Ku Park, Il Suh, Tae-Yong Lee
Clinical Hypertension.2024;[Epub] CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Effect of Adding Apolipoprotein B Testing on the Prevalence of Dyslipidemia and Risk of Cardiovascular Disease in the Korean Adult Population
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Metabolites.2024; 14(3): 169. CrossRef - A self-powered and supercapacitive microneedle continuous glucose monitoring system with a wide range of glucose detection capabilities
Hye-Jun Kil, Jang Hyeon Kim, Kanghae Lee, Tae-Uk Kang, Ju-Hyun Yoo, Yong-ho Lee, Jin-Woo Park
Biosensors and Bioelectronics.2024; 257: 116297. CrossRef - Cardiorenal outcomes and mortality after sodium‐glucose cotransporter‐2 inhibitor initiation in type 2 diabetes patients with percutaneous coronary intervention history
Jin Hwa Kim, Young Sang Lyu, BongSeong Kim, Mee Kyung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Recommendations for Pharmacological Treatment of Type 2 Diabetes
Junghyun Noh
The Journal of Korean Diabetes.2023; 24(3): 127. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - A 33-Year-Old Man Presented with Abdominal Pain and Vomiting Starting a Day Ago
Jong Han Choi
The Korean Journal of Medicine.2023; 98(6): 289. CrossRef - Comorbidity Patterns and Management in Inpatients with Endocrine Diseases by Age Groups in South Korea: Nationwide Data
Sung-Soo Kim, Hun-Sung Kim
Journal of Personalized Medicine.2023; 14(1): 42. CrossRef
- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
- Technology/Device
- Clinical and Lifestyle Determinants of Continuous Glucose Monitoring Metrics in Insulin-Treated Patients with Type 2 Diabetes Mellitus
- Da Young Lee, Namho Kim, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Jihee Kim, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Sung-Min Park, Nan Hee Kim
- Diabetes Metab J. 2023;47(6):826-836. Published online August 24, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0273
- 1,790 View
- 191 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
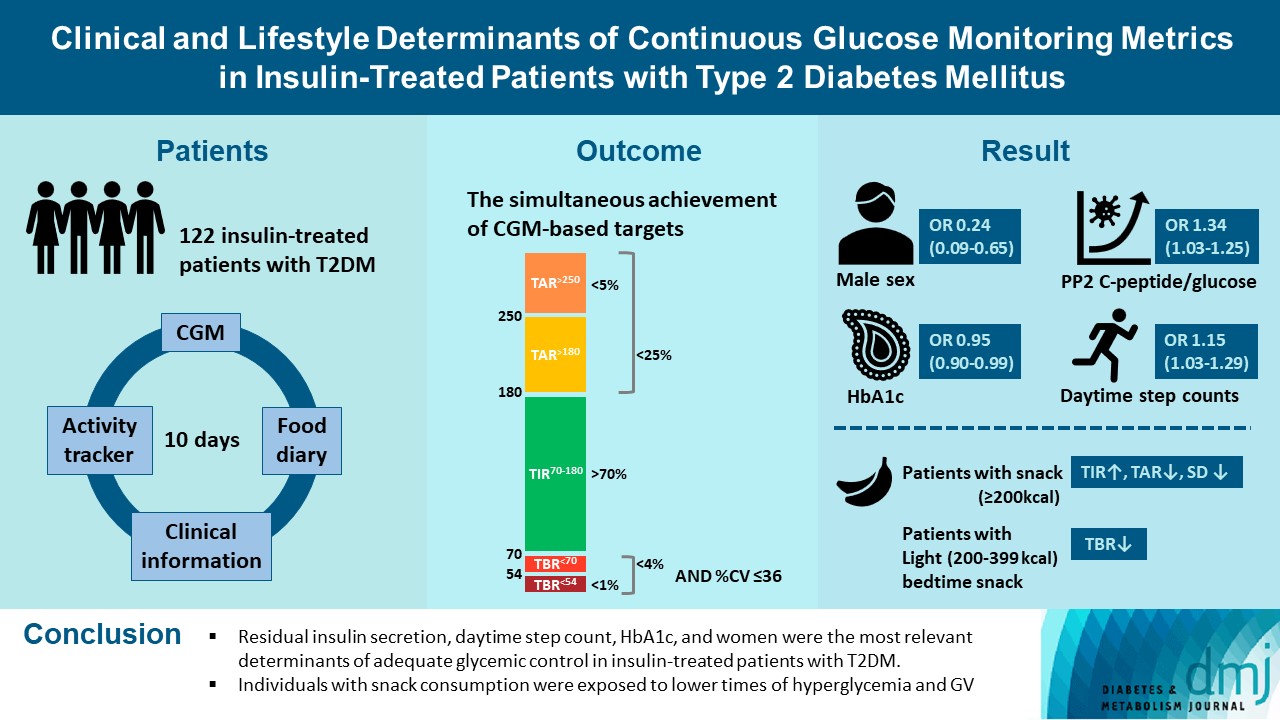
There was limited evidence to evaluate the association between lifestyle habits and continuous glucose monitoring (CGM) metrics. Thus, we aimed to depict the behavioral and metabolic determinants of CGM metrics in insulin-treated patients with type 2 diabetes mellitus (T2DM).
Methods
This is a prospective observational study. We analyzed data from 122 insulin-treated patients with T2DM. Participants wore Dexcom G6 and Fitbit, and diet information was identified for 10 days. Multivariate-adjusted logistic regression analysis was performed for the simultaneous achievement of CGM-based targets, defined by the percentage of time in terms of hyper, hypoglycemia and glycemic variability (GV). Intake of macronutrients and fiber, step counts, sleep, postprandial C-peptide-to-glucose ratio (PCGR), information about glucose lowering medications and metabolic factors were added to the analyses. Additionally, we evaluated the impact of the distribution of energy and macronutrient during a day, and snack consumption on CGM metrics.
Results
Logistic regression analysis revealed that female, participants with high PCGR, low glycosylated hemoglobin (HbA1c) and daytime step count had a higher probability of achieving all targets based on CGM (odds ratios [95% confidence intervals] which were 0.24 [0.09 to 0.65], 1.34 [1.03 to 1.25], 0.95 [0.9 to 0.99], and 1.15 [1.03 to 1.29], respectively). And participants who ate snacks showed a shorter period of hyperglycemia and less GV compared to those without.
Conclusion
We confirmed that residual insulin secretion, daytime step count, HbA1c, and women were the most relevant determinants of adequate glycemic control in insulin-treated patients with T2DM. In addition, individuals with snack consumption were exposed to lower times of hyperglycemia and GV. -
Citations
Citations to this article as recorded by- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
Lotte Bogaert, Iris Willems, Patrick Calders, Eveline Dirinck, Manon Kinaupenne, Marga Decraene, Bruno Lapauw, Boyd Strumane, Margot Van Daele, Vera Verbestel, Marieke De Craemer
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2024; 18(4): 102995. CrossRef
- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
- Others
- Fasting Glucose Variability and the Risk of Dementia in Individuals with Diabetes: A Nationwide Cohort Study
- Da Young Lee, Jaeyoung Kim, Sanghyun Park, So Young Park, Ji Hee Yu, Ji A Seo, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Kyungdo Han, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):923-935. Published online May 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0346
- 5,609 View
- 254 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated whether fasting glucose (FG) variability could predict the risk of dementia.
Methods
This cohort study analyzed data from Koreans with diabetes after at least three health examinations by the Korean National Health Insurance Corporation between 2005 and 2010, which included at least one examination between 2009 and 2010. A total of 769,554 individuals were included, excluding those aged <40 years and those with dementia. FG variability was measured using the variability independent of the mean (FG-VIM). The incidence of dementia was defined by the International Classification of Diseases 10th Revision codes and prescription of anti-dementia medication and was subdivided into Alzheimer’s disease (AD) and vascular dementia (VD).
Results
During the 6.9-year follow-up, 54,837, 41,032, and 6,892 cases of all-cause dementia, AD, and VD, respectively, were identified. Cox proportional regression analyses showed that as the FG-VIM quartile increased, the risk of dementia serially increased after adjustment for metabolic factors, income status, and diabetes-related characteristics, including the mean FG. Participants in FG-VIM quartile 4 showed a 18%, 19%, and 17% higher risk for all-cause dementia, AD, and VD, respectively, than those in quartile 1; this particularly included non-obese patients with a longer duration of diabetes, high FG levels, dyslipidemia, and those taking glucose-lowering medications. Conversely, the baseline FG status and dementia showed a U-shaped association.
Conclusion
Increased FG variability over 5 years can predict the risk of dementia in individuals with diabetes in Korea. This finding was more pronounced in patients with less favorable metabolic profiles. -
Citations
Citations to this article as recorded by- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
Sung Hoon Kang, Yunjin Choi, Su Jin Chung, Seok-Joo Moon, Chi Kyung Kim, Ji Hyun Kim, Kyungmi Oh, Joon Shik Yoon, Sang Won Seo, Geum Joon Cho, Seong-Beom Koh
Frontiers in Aging Neuroscience.2024;[Epub] CrossRef - Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
Vishal Chavda, Dhananjay Yadav, Snehal Patel, Minseok Song
Brain Sciences.2024; 14(3): 284. CrossRef - The Association of Glucose Variability and Dementia Incidence in Latinx Adults with Type 2 Diabetes: A Retrospective Study
Heather Cuevas, Elizabeth Muñoz, Divya Nagireddy, Jeeyeon Kim, Grace Ganucheau, Fathia Alomoush
Clinical Nursing Research.2023; 32(2): 249. CrossRef - The effects of long-term cumulative HbA1c exposure on the development and onset time of dementia in the patients with type 2 diabetes mellitus: Hospital based retrospective study (2005–2021)
Sunyoung Cho, Choon Ok Kim, Bong-soo Cha, Eosu Kim, Chung Mo Nam, Min-Gul Kim, Min Soo Park
Diabetes Research and Clinical Practice.2023; 201: 110721. CrossRef - Physiological Mechanisms Inherent to Diabetes Involved in the Development of Dementia: Alzheimer’s Disease
Himan Mohamed-Mohamed, Victoria García-Morales, Encarnación María Sánchez Lara, Anabel González-Acedo, Teresa Pardo-Moreno, María Isabel Tovar-Gálvez, Lucía Melguizo-Rodríguez, Juan José Ramos-Rodríguez
Neurology International.2023; 15(4): 1253. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef
- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
- Technology/Device
- Comparison of Laser and Conventional Lancing Devices for Blood Glucose Measurement Conformance and Patient Satisfaction in Diabetes Mellitus
- Jung A Kim, Min Jeong Park, Eyun Song, Eun Roh, So Young Park, Da Young Lee, Jaeyoung Kim, Ji Hee Yu, Ji A Seo, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):936-940. Published online March 30, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0293
- 5,272 View
- 256 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Self-monitoring of capillary blood glucose is important for controlling diabetes. Recently, a laser lancing device (LMT-1000) that can collect capillary blood without skin puncture was developed. We enrolled 150 patients with type 1 or 2 diabetes mellitus. Blood sampling was performed on the same finger on each hand using the LMT-1000 or a conventional lancet. The primary outcome was correlation between glucose values using the LMT-1000 and that using a lancet. And we compared the pain and satisfaction of the procedures. The capillary blood sampling success rates with the LMT-1000 and lancet were 99.3% and 100%, respectively. There was a positive correlation (r=0.974, P<0.001) between mean blood glucose levels in the LMT-1000 (175.8±63.0 mg/dL) and conventional lancet samples (172.5±63.6 mg/dL). LMT-1000 reduced puncture pain by 75.0% and increased satisfaction by 80.0% compared to a lancet. We demonstrated considerable consistency in blood glucose measurements between samples from the LMT-1000 and a lancet, but improved satisfaction and clinically significant pain reduction were observed with the LMT-1000 compared to those with a lancet.
-
Citations
Citations to this article as recorded by- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
Chul Kyu Yun, Eui Kyung Choi, Hyung Jin Kim, Jaeyoung Kim, Byung Cheol Park, Kyuhee Park, Byung Min Choi
Journal of Perinatology.2024;[Epub] CrossRef
- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
- Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
- Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
- Diabetes Metab J. 2021;45(4):617-618. Published online July 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0152
- 3,831 View
- 99 Download
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- The effect of close and intensive therapeutic monitoring of patients with poorly controlled type 2 diabetes with different glycemic background
Ayşe Naciye Erbakan, Müzeyyen Arslan Bahadir, Fatoş Nimet Kaya, Büşra Güleç, Miraç Vural Keskinler, Özge Faydaliel, Banu Mesçi, Aytekin Oğuz
Medicine.2023; 102(50): e36680. CrossRef - Reduced macula microvascular densities may be an early indicator for diabetic peripheral neuropathy
Xiaoyu Deng, Shiqi Wang, Yan Yang, Aizhen Chen, Jinger Lu, Jinkui Hao, Yufei Wu, Qinkang Lu
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef
- The effect of close and intensive therapeutic monitoring of patients with poorly controlled type 2 diabetes with different glycemic background
- Skeletal Muscle Should Not Be Overlooked
- Ji A Seo
- Diabetes Metab J. 2021;45(2):173-174. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0024
- 3,285 View
- 123 Download
- Complications
-
- Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study
- Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
- Diabetes Metab J. 2021;45(3):368-378. Published online October 20, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0046

- 9,380 View
- 343 Download
- 19 Web of Science
- 19 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
To evaluate the association of time to reach the target glycosylated hemoglobin (HbA1c) level with long-term durable glycemic control and risk of diabetic complications in patients with newly diagnosed type 2 diabetes mellitus (T2DM).
Methods
In a longitudinal observational cohort, 194 patients with T2DM newly diagnosed between January 2011 and March 2013 were followed up over 6 years. Patients were classified according to the time needed to reach the target HbA1c (<7.0%): <3, 3 to 6 (early achievement group), and ≥6 months (late achievement group). Risks of microvascular complications including diabetic retinopathy, nephropathy, and neuropathy as well as macrovascular events including ischemic heart disease, ischemic stroke, and peripheral arterial disease were assessed by multivariable Cox proportional hazards analysis.
Results
During a median follow-up of 6.53 years, 66 microvascular and 14 macrovascular events occurred. Maintenance of durable glycemic control over 6 years was more likely in the early achievement groups than in the late achievement group (34.5%, 30.0%, and 16.1% in <3, 3 to 6, and ≥6 months, respectively, P=0.039). Early target HbA1c achievement was associated with lower risk of composite diabetic complications (adjusted hazard ratio [HR, 0.47; 95% confidence interval [CI], 0.26 to 0.86 in <3 months group) (adjusted HR, 0.50; 95% CI, 0.23 to 1.10 in 3 to 6 months group, in reference to ≥6 months group). Similar trends were maintained for risks of microvascular and macrovascular complications, although statistical significance was not reached for macrovascular complications.
Conclusion
Early target HbA1c achievement was associated with long-term durable glycemic control and reduced risk of diabetic complications in newly diagnosed T2DM. -
Citations
Citations to this article as recorded by- HbA1c As Diabetes Mellitus Biomarker and Its Methods Evolution
Liong Boy Kurniawan
INDONESIAN JOURNAL OF CLINICAL PATHOLOGY AND MEDICAL LABORATORY.2024; 30(2): 191. CrossRef - Efficacy and safety of enavogliflozin vs. dapagliflozin as add-on therapy in patients with type 2 diabetes mellitus based on renal function: a pooled analysis of two randomized controlled trials
Young Sang Lyu, Sangmo Hong, Si Eun Lee, Bo Young Cho, Cheol-Young Park
Cardiovascular Diabetology.2024;[Epub] CrossRef - The effect of health quotient and time management skills on self-management behavior and glycemic control among individuals with type 2 diabetes mellitus
Mengjie Chen, Man Liu, Ying Pu, Juan Wu, Mingjiao Zhang, Hongxia Tang, Laixi Kong, Maoting Guo, Kexue Zhu, Yuxiu Xie, Zhe Li, Bei Deng, Zhenzhen Xiong
Frontiers in Public Health.2024;[Epub] CrossRef - Glycemic control and cardiovascular complications of type 2 diabetes mellitus
I. V. Druk, S. S. Safronova
Meditsinskiy sovet = Medical Council.2023; (13): 130. CrossRef - Effect of viscous soluble dietary fiber on glucose and lipid metabolism in patients with type 2 diabetes mellitus: a systematic review and meta-analysis on randomized clinical trials
Kun Lu, Tingqing Yu, Xinyi Cao, Hui Xia, Shaokang Wang, Guiju Sun, Liang Chen, Wang Liao
Frontiers in Nutrition.2023;[Epub] CrossRef - Construction and validation of a clinical prediction model for asymptomatic obstructive coronary stenosis in patients with carotid stenosis
Cuijie Qin, Chuang Li, Yunpeng Luo, Zhen Li, Hui Cao
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Risk assessment of rectal anastomotic leakage (RAREAL) after DIXON in non-emergency patients with rectal cancer
Xue-Cong Zheng, Jin-Bo Su, Jin-Jie Zheng
BMC Gastroenterology.2023;[Epub] CrossRef - Evaluation of Left Ventricular Function in Diabetes Patients with Microvascular Disease by Three-Dimensional Speckle Tracking Imaging
青 周
Advances in Clinical Medicine.2023; 13(12): 18908. CrossRef - Validity of the diagnosis of diabetic microvascular complications in Korean national health insurance claim data
Hyung Jun Kim, Moo-Seok Park, Jee-Eun Kim, Tae-Jin Song
Annals of Clinical Neurophysiology.2022; 24(1): 7. CrossRef - Metformin plus a low hypoglycemic risk antidiabetic drug vs. metformin monotherapy for untreated type 2 diabetes mellitus: A meta-analysis of randomized controlled trials
Wei-Tse Hung, Yuan-Jung Chen, Chun-Yu Cheng, Bruce Ovbiagele, Meng Lee, Chia-Yu Hsu
Diabetes Research and Clinical Practice.2022; 189: 109937. CrossRef - Peripheral arterial disease progression and ankle brachial index: a cohort study with newly diagnosed patients with type 2 diabetes
João Soares Felício, Franciane Trindade Cunha de Melo, Giovana Miranda Vieira, Vitória Teixeira de Aquino, Fernanda de Souza Parente, Wanderson Maia da Silva, Nivin Mazen Said, Emanuele Rocha da Silva, Ana Carolina Contente Braga de Souza, Maria Clara Ner
BMC Cardiovascular Disorders.2022;[Epub] CrossRef - Association of long-term visit-to-visit variability of HbA1c and fasting glycemia with hypoglycemia in type 2 diabetes mellitus
Chen Long, Yaling Tang, Jiangsheng Huang, Suo Liu, Zhenhua Xing
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Degree of Glycemic Control for the First Three Months Determines the Next Seven Years
Nami Lee, Dae Jung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Inhibition of advanced glycation end products and protein oxidation by leaf extracts and phenolics from Chilean bean landraces
Felipe Ávila, Nadia Cruz, Jazmin Alarcon-Espósito, Nélida Nina, Hernán Paillan, Katherine Márquez, Denis Fuentealba, Alberto Burgos-Edwards, Cristina Theoduloz, Carmina Vejar-Vivar, Guillermo Schmeda-Hirschmann
Journal of Functional Foods.2022; 98: 105270. CrossRef - Mediation Effect of Self-Efficacy Between Health Beliefs and Glycated Haemoglobin Levels in Elderly Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study
Anqi Zhang, Jinsong Wang, Xiaojuan Wan, Jing Zhang, Zihe Guo, Yamin Miao, Shuhan Zhao, Shuo Bai, Ziyi Zhang, Weiwei Yang
Patient Preference and Adherence.2022; Volume 16: 3015. CrossRef - Early Glycosylated Hemoglobin Target Achievement Predicts Clinical Outcomes in Patients with Newly Diagnosed Type 2 Diabetes Mellitus
Joonyub Lee, Jae Hyoung Cho
Diabetes & Metabolism Journal.2021; 45(3): 337. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
Ja Young Jeon
Diabetes & Metabolism Journal.2021; 45(4): 613. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2021; 45(4): 617. CrossRef - Plasma Nesfatin-1: Potential Predictor and Diagnostic Biomarker for Cognitive Dysfunction in T2DM Patient
Dandan Xu, Yue Yu, Yayun Xu, Jinfang Ge
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 3555. CrossRef
- HbA1c As Diabetes Mellitus Biomarker and Its Methods Evolution
- Metabolic Risk/Epidemiology
- Age- and Sex-Related Differential Associations between Body Composition and Diabetes Mellitus
- Eun Roh, Soon Young Hwang, Jung A Kim, You-Bin Lee, So-hyeon Hong, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
- Diabetes Metab J. 2021;45(2):183-194. Published online June 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0171

- 7,440 View
- 236 Download
- 3 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
Background The age- and sex-related differences on the impacts of body composition on diabetes mellitus (DM) remain uncertain.
Methods The fourth and fifth Korea National Health and Nutrition Examination Survey included 15,586 subjects over 30 years of age who completed dual-energy X-ray absorptiometry. We conducted a cross-sectional study to investigate whether muscle mass index (MMI), defined as appendicular skeletal muscle divided by body mass index (BMI), and fat mass index (FMI), defined as trunk fat mass divided by BMI, were differently associated with DM according to age and sex.
Results In multivariate logistic regression, the risk for DM significantly increased across quartiles of FMI in men aged ≥70. Meanwhile, MMI showed a protective association with DM in men of the same age. The odds ratios (ORs) for the highest quartile versus the lowest quartile of FMI and MMI were 3.116 (95% confidence interval [CI], 1.405 to 6.914) and 0.295 (95% CI, 0.157 to 0.554), respectively. In women, the ORs of DM was significantly different across FMI quartiles in those over age 50. The highest quartile of FMI exhibited increased ORs of DM in subjects aged 50 to 69 (OR, 1.891; 95% CI, 1.229 to 2.908) and ≥70 (OR, 2.275; 95% CI, 1.103 to 4.69) compared to lowest quartile. However, MMI was not significantly associated with DM in women of all age groups.
Conclusion Both FMI and MMI were independent risk factors for DM in men aged 70 years or more. In women over 50 years, FMI was independently associated with DM. There was no significant association between MMI and DM in women.
-
Citations
Citations to this article as recorded by- Research Progress on Correlation between Body Composition Changes and Disease Pro-gression of Type 2 Diabetes
敏 张
Advances in Clinical Medicine.2024; 14(03): 936. CrossRef - Low Skeletal Muscle Mass Accompanied by Abdominal Obesity Additively Increases the Risk of Incident Type 2 Diabetes
Ji Eun Jun, Seung-Eun Lee, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hwan Jee, Jae Hyeon Kim
The Journal of Clinical Endocrinology & Metabolism.2023; 108(5): 1173. CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Whole and segmental body composition changes during mid-follicular and mid-luteal phases of the menstrual cycle in recreationally active young women
Şükran Nazan Koşar, Yasemin Güzel, Mehmet Gören Köse, Ayşe Kin İşler, Tahir Hazır
Annals of Human Biology.2022; 49(2): 124. CrossRef - Body Composition and Diabetes
Hye Jin Yoo
The Journal of Korean Diabetes.2021; 22(4): 238. CrossRef
- Research Progress on Correlation between Body Composition Changes and Disease Pro-gression of Type 2 Diabetes
- Clinical Complications
- Incidence and Risk Factors for Dementia in Type 2 Diabetes Mellitus: A Nationwide Population-Based Study in Korea
- Ji Hee Yu, Kyungdo Han, Sanghyun Park, Hanna Cho, Da Young Lee, Jin-Wook Kim, Ji A Seo, Sin Gon Kim, Sei Hyun Baik, Yong Gyu Park, Kyung Mook Choi, Seon Mee Kim, Nan Hee Kim
- Diabetes Metab J. 2020;44(1):113-124. Published online November 12, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0216
- 7,856 View
- 197 Download
- 31 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Diabetes mellitus is associated with an increased risk of dementia. We aimed to comprehensively analyze the incidence and risk factors for dementia and young-onset dementia (YOD) in diabetic patients in Korea using the National Health Insurance Service data.
Methods Between January 1, 2009 and December 31, 2012, a total of 1,917,702 participants with diabetes were included and followed until the date of dementia diagnosis or until December 31, 2015. We evaluated the incidence and risk factors for all dementia, Alzheimer's disease (AD), and vascular dementia (VaD) by Cox proportional hazards analyses. We also compared the impact of risk factors on the occurrence of YOD and late-onset dementia (LOD).
Results During an average of 5.1 years of follow-up, the incidence of all types of dementia, AD, or VaD was 9.5, 6.8, and 1.3/1,000 person-years, respectively, in participants with diabetes. YOD comprised 4.8% of all dementia occurrence, and the ratio of AD/VaD was 2.1 for YOD compared with 5.5 for LOD. Current smokers and subjects with lower income, plasma glucose levels, body mass index (BMI), and subjects with hypertension, dyslipidemia, vascular complications, depression, and insulin treatment developed dementia more frequently. Vascular risk factors such as smoking, hypertension, and previous cardiovascular diseases were more strongly associated with the development of VaD than AD. Low BMI and a history of stroke or depression had a stronger influence on the development of YOD than LOD.
Conclusion The optimal management of modifiable risk factors may be important for preventing dementia in subjects with diabetes mellitus.
-
Citations
Citations to this article as recorded by- Unlocking the Protective Potential of Upper Respiratory Infection Treatment Histories against Alzheimer’s Disease: A Korean Adult Population Study
Ho Suk Kang, Ji Hee Kim, Joo-Hee Kim, Woo Jin Bang, Hyo Geun Choi, Nan Young Kim, Ha Young Park, Mi Jung Kwon
Journal of Clinical Medicine.2024; 13(1): 260. CrossRef - Hepatopancreatic metabolic disorders and their implications in the development of Alzheimer's disease and vascular dementia
Francisco I. Pinheiro, Irami Araújo-Filho, Amália C.M. do Rego, Eduardo P. de Azevedo, Ricardo N. Cobucci, Fausto P. Guzen
Ageing Research Reviews.2024; 96: 102250. CrossRef - Amygdala activity and amygdala-hippocampus connectivity: Metabolic diseases, dementia, and neuropsychiatric issues
Juhyun Song
Biomedicine & Pharmacotherapy.2023; 162: 114647. CrossRef - The effects of long-term cumulative HbA1c exposure on the development and onset time of dementia in the patients with type 2 diabetes mellitus: Hospital based retrospective study (2005–2021)
Sunyoung Cho, Choon Ok Kim, Bong-soo Cha, Eosu Kim, Chung Mo Nam, Min-Gul Kim, Min Soo Park
Diabetes Research and Clinical Practice.2023; 201: 110721. CrossRef - Association of triglyceride/high-density lipoprotein cholesterol ratio with severe complications of COVID-19
Yoonkyung Chang, Jimin Jeon, Tae-Jin Song, Jinkwon Kim
Heliyon.2023; 9(6): e17428. CrossRef - Akkermansia muciniphila in neuropsychiatric disorders: friend or foe?
Wenhui Lei, Yiwen Cheng, Jie Gao, Xia Liu, Li Shao, Qingming Kong, Nengneng Zheng, Zongxin Ling, Weiming Hu
Frontiers in Cellular and Infection Microbiology.2023;[Epub] CrossRef - The Association Between Eye Disease and Incidence of Dementia: Systematic Review and Meta-Analysis
Jiayi Feng, Cuihong Huang, Lei Liang, Chuang Li, Xiaojie Wang, Jianping Ma, Xinhui Guan, Bin Jiang, Shaofen Huang, Pei Qin
Journal of the American Medical Directors Association.2023; 24(9): 1363. CrossRef - Risk of Neurodegenerative Diseases in Elderly Koreans with an Initial Diagnosis of Type 2 Diabetes: A Nationwide Retrospective Cohort Study
Hee-Cheol Kim, Ho-Jun Lee, Yang-Tae Kim, Byeong-Churl Jang, Asirvatham Alwin Robert
Journal of Diabetes Research.2023; 2023: 1. CrossRef - Type-2 Diabetes Alters Hippocampal Neural Oscillations and Disrupts Synchrony between the Hippocampus and Cortex
Gratianne Rabiller, Zachary Ip, Shahram Zarrabian, Hongxia Zhang, Yoshimichi Sato, Azadeh Yazdan-Shahmorad, Jialing Liu
Aging and disease.2023;[Epub] CrossRef - Sarcopenia and diabetes-induced dementia risk
Mingyang Sun, Zhongyuan Lu, Wan-Ming Chen, Szu-Yuan Wu, Jiaqiang Zhang
Brain Communications.2023;[Epub] CrossRef - Association of periodontitis with microvascular complications of diabetes mellitus: A nationwide cohort study
Moo-Seok Park, Jimin Jeon, Tae-Jin Song, Jinkwon Kim
Journal of Diabetes and its Complications.2022; 36(2): 108107. CrossRef - Association between oral health and cardiovascular outcomes in patients with hypertension: a nationwide cohort study
Jinkwon Kim, Hyung Jun Kim, Jimin Jeon, Tae-Jin Song
Journal of Hypertension.2022; 40(2): 374. CrossRef - Diabetic retinopathy and cognitive dysfunction: a systematic review and meta-analysis
Mei Wu, Fan Mei, Kaiyan Hu, Liyuan Feng, Zhe Wang, Qianqian Gao, Fei Chen, Li Zhao, Xiaohui Li, Bin Ma
Acta Diabetologica.2022; 59(4): 443. CrossRef - Associations between depression and cognition, mild cognitive impairment and dementia in persons with diabetes mellitus: A systematic review and meta-analysis
Yeng Yan Chow, Milou Verdonschot, Claire T. McEvoy, Geeske Peeters
Diabetes Research and Clinical Practice.2022; 185: 109227. CrossRef - Diabetes Mellitus: A Path to Amnesia, Personality, and Behavior Change
Rahnuma Ahmad, Kona Chowdhury, Santosh Kumar, Mohammed Irfan, Govindool Reddy, Farhana Akter, Dilshad Jahan, Mainul Haque
Biology.2022; 11(3): 382. CrossRef - Hypothyroidism and Diabetes-Related Dementia: Focused on Neuronal Dysfunction, Insulin Resistance, and Dyslipidemia
Hee Kyung Kim, Juhyun Song
International Journal of Molecular Sciences.2022; 23(6): 2982. CrossRef - Type 2 Diabetes Mellitus as a Risk Factor for Alzheimer’s Disease: Review and Meta-Analysis
Athanasia Athanasaki, Konstantinos Melanis, Ioanna Tsantzali, Maria Ioanna Stefanou, Sofia Ntymenou, Sotirios G. Paraskevas, Theodosis Kalamatianos, Eleni Boutati, Vaia Lambadiari, Konstantinos I. Voumvourakis, George Stranjalis, Sotirios Giannopoulos, Ge
Biomedicines.2022; 10(4): 778. CrossRef - Cardiometabolic measures and cognition in early menopause - Analysis of baseline data from a randomized controlled trial
Lubna Pal, Kelly Morgan, Nanette F. Santoro, JoAnn E. Manson, Hugh S. Taylor, Virginia M. Miller, Eliot A. Brinton, Rogerio Lobo, Genevieve Neal-Perry, Marcelle I. Cedars, S. Mitchell Harman, Taryn T. James, Carey E. Gleason
Maturitas.2022; 162: 58. CrossRef - Dysfunctional Glucose Metabolism in Alzheimer’s Disease Onset and Potential Pharmacological Interventions
Vijay Kumar, So-Hyeon Kim, Kausik Bishayee
International Journal of Molecular Sciences.2022; 23(17): 9540. CrossRef - Metabolically healthy obesity: it is time to consider its dynamic changes
Yun Kyung Cho, Chang Hee Jung
Cardiovascular Prevention and Pharmacotherapy.2022; 4(4): 123. CrossRef - Association between cholesterol levels and dementia risk according to the presence of diabetes and statin use: a nationwide cohort study
You-Bin Lee, Min Young Kim, Kyungdo Han, Bongsung Kim, Jiyun Park, Gyuri Kim, Kyu Yeon Hur, Jae Hyeon Kim, Sang-Man Jin
Scientific Reports.2022;[Epub] CrossRef - The insulin resistance by triglyceride glucose index and risk for dementia: population-based study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
Alzheimer's Research & Therapy.2021;[Epub] CrossRef - The identification of established modifiable mid-life risk factors for cardiovascular disease which contribute to cognitive decline: Korean Longitudinal Study of Aging (KLoSA)
Yebeen Ysabelle Boo, Otto-Emil Jutila, Meghan A. Cupp, Logan Manikam, Sung-Il Cho
Aging Clinical and Experimental Research.2021; 33(9): 2573. CrossRef - Examining the effects of multiple chronic conditions on cognitive decline and potential moderators among older Koreans: Findings from the Korean Longitudinal Study of Ageing 2006–2016
Yura Lee, Chi C. Cho
Archives of Gerontology and Geriatrics.2021; 95: 104424. CrossRef - Cumulative Exposure to Metabolic Syndrome Components and the Risk of Dementia: A Nationwide Population-Based Study
Yunjung Cho, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2021; 36(2): 424. CrossRef - Cardiovascular risks of periodontitis and oral hygiene indicators in patients with diabetes mellitus
Tae-Jin Song, Jimin Jeon, Jinkwon Kim
Diabetes & Metabolism.2021; 47(6): 101252. CrossRef - Association Between Diabetic Retinopathy and Cognitive Impairment: A Systematic Review and Meta-Analysis
Dihe Cheng, Xue Zhao, Shuo Yang, Guixia Wang, Guang Ning
Frontiers in Aging Neuroscience.2021;[Epub] CrossRef - Improving Cognition with Nutraceuticals Targeting TGF-β1 Signaling
Margherita Grasso, Giuseppe Caruso, Justyna Godos, Angela Bonaccorso, Claudia Carbone, Sabrina Castellano, Walter Currenti, Giuseppe Grosso, Teresa Musumeci, Filippo Caraci
Antioxidants.2021; 10(7): 1075. CrossRef - The risk of Alzheimer’s disease according to dynamic changes in metabolic health and obesity: a nationwide population-based cohort study
Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Joong-Yeol Park, Woo Je Lee, Ye-Jee Kim, Chang Hee Jung
Aging.2021; 13(13): 16974. CrossRef - Letter: Hypoglycemia and Dementia Risk in Older Patients with Type 2 Diabetes Mellitus: A Propensity-Score Matched Analysis of a Population-Based Cohort Study (Diabetes Metab J 2020;44:125–33)
Jin Hwa Kim
Diabetes & Metabolism Journal.2020; 44(2): 356. CrossRef - The Interplay between Diabetes and Alzheimer’s Disease—In the Hunt for Biomarkers
Adriana Kubis-Kubiak, Aleksandra Dyba, Agnieszka Piwowar
International Journal of Molecular Sciences.2020; 21(8): 2744. CrossRef - Association between cytomegalovirus end-organ diseases and moderate-to-severe dementia: a population-based cohort study
Kyoung Hwa Lee, Da Eun Kwon, Kyung Do Han, Yeonju La, Sang Hoon Han
BMC Neurology.2020;[Epub] CrossRef
- Unlocking the Protective Potential of Upper Respiratory Infection Treatment Histories against Alzheimer’s Disease: A Korean Adult Population Study
- Clinical Diabetes & Therapeutics
- An Age of Sodium-Glucose Cotransporter-2 Inhibitor Priority: Are We Ready?
- Ji A Seo
- Diabetes Metab J. 2019;43(5):578-581. Published online October 24, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0173
- 3,130 View
- 35 Download
- Obesity and Metabolic Syndrome
- Proportion and Characteristics of the Subjects with Low Muscle Mass and Abdominal Obesity among the Newly Diagnosed and Drug-Naïve Type 2 Diabetes Mellitus Patients
- Jung A Kim, Soon Young Hwang, Hye Soo Chung, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
- Diabetes Metab J. 2019;43(1):105-113. Published online September 28, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0036
- 4,894 View
- 70 Download
- 12 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Sarcopenic obesity (SO) is a serious public health concern, few studies have examined the clinical implications of SO in newly-diagnosed type 2 diabetes mellitus (T2DM) patients. We evaluated the prevalence of the newly diagnosed, drug-naïve T2DM patients with low muscle mass with abdominal obesity and its association with insulin resistance and other diabetic complications.
Methods We classified 233 drug-naïve T2DM subjects into four groups according to abdominal obesity (waist circumference ≥90 cm in men and ≥85 cm in women) and low muscle mass status (appendicular skeletal muscle <7.0 kg/m2 for men and <5.4 kg/m2 for women).
Results The proportion of the subjects with low muscle mass and abdominal obesity among the newly diagnosed, drug-naïve T2DM patients was 8.2%. Homeostasis model assessment of insulin resistance (HOMA-IR) increased linearly according to body composition group from normal to abdominal obesity to both low muscle mass and abdominal obesity. The multiple logistic regression analysis indicated that subjects with low muscle mass and abdominal obesity (odds ratio [OR], 9.39; 95% confidence interval [CI], 2.41 to 36.56) showed a higher risk for insulin resistance, defined as HOMA-IR ≥3, than those with abdominal obesity (OR, 5.36; 95% CI, 2.46 to 11.69), even after adjusting for other covariates. However, there were no differences in lipid profiles, microalbuminuria, or various surrogate markers for atherosclerosis among the four groups.
Conclusion Subjects with both low muscle mass and abdominal obesity had a higher risk of insulin resistance than those with low muscle mass or abdominal obesity only.
-
Citations
Citations to this article as recorded by- Clinical observation on acupuncture for 80 patients with abdominal obesity in Germany: based on the theory of unblocking and regulating the Belt Vessel
Yuanyuan Li, Hang Xiong, Shuhui Ma, Jingzhang Dai
Journal of Acupuncture and Tuina Science.2023; 21(2): 137. CrossRef - Waist circumference and end‐stage renal disease based on glycaemic status: National Health Insurance Service data 2009–2018
Yun Kyung Cho, Ji Hye Huh, Shinje Moon, Yoon Jung Kim, Yang‐Hyun Kim, Kyung‐do Han, Jun Goo Kang, Seong Jin Lee, Sung‐Hee Ihm
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 585. CrossRef - Incidence of sarcopenic obesity in older patients with diabetes and association between sarcopenic obesity and higher-level functional capacity: evaluation based on a consensus statement
Satoshi Ida, Ryutaro Kaneko, Kanako Imataka, Kaoru Okubo, Kentaro Azuma, Kazuya Murata
Endocrine Journal.2023; 70(6): 591. CrossRef - A Novel Anthropometric Parameter, Weight-Adjusted Waist Index Represents Sarcopenic Obesity in Newly Diagnosed Type 2 Diabetes Mellitus
Min Jeong Park, Soon Young Hwang, Nam Hoon Kim, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 130. CrossRef - Prevalence of sarcopenic obesity in patients with diabetes and adverse outcomes: A systematic review and meta-analysis
Yuan-yuan Zhou, Jin-feng Wang, Qian Yao, Qiu-feng Jian, Zhi-peng Luo
Clinical Nutrition ESPEN.2023; 58: 128. CrossRef - The Correlation Between Leg Muscle Mass Index and Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus
Menggege Liu, Qing Zhang, Juan Liu, Huiling Bai, Ping Yang, Xinhua Ye, Xiaoqing Yuan
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 4169. CrossRef - Sarcopenic Obesity with Normal Body Size May Have Higher Insulin Resistance in Elderly Patients with Type 2 Diabetes Mellitus
Tingting Han, Ting Yuan, Xinyue Liang, Ningxin Chen, Jia Song, Xin Zhao, Yurong Weng, Yaomin Hu
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 1197. CrossRef - Relationship between Visceral Adipose Index, Lipid Accumulation Product and Type 2 Diabetes Mellitus
停停 陈
Advances in Clinical Medicine.2022; 12(04): 3350. CrossRef - Assessment of the relationship between prediabetes and low skeletal mass based on blood creatinine level
S. I. Ibragimova, G. O. Nuskabayeva, Z. N. Shalkharova, K. Zh. Sadykova, G. A. Junusbekova, M. Oran
Diabetes mellitus.2022; 25(3): 226. CrossRef - Changes in body composition and low blood urea nitrogen level related to an increase in the prevalence of fatty liver over 20 years: A cross‐sectional study
Yasushi Imamura, Seiichi Mawatari, Kohei Oda, Kotaro Kumagai, Yasunari Hiramine, Akiko Saishoji, Atsuko Kakihara, Mai Nakahara, Manei Oku, Kaori Hosoyamada, Shuji Kanmura, Akihiro Moriuchi, Hironori Miyahara, Akio ido
Hepatology Research.2021; 51(5): 570. CrossRef - Body Composition and Diabetes
Hye Jin Yoo
The Journal of Korean Diabetes.2021; 22(4): 238. CrossRef - Reduced Skeletal Muscle Volume and Increased Skeletal Muscle Fat Deposition Characterize Diabetes in Individuals after Pancreatitis: A Magnetic Resonance Imaging Study
Andre E. Modesto, Juyeon Ko, Charlotte E. Stuart, Sakina H. Bharmal, Jaelim Cho, Maxim S. Petrov
Diseases.2020; 8(3): 25. CrossRef - Low alanine aminotransferase levels predict low muscle strength in older patients with diabetes: A nationwide cross‐sectional study in Korea
Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Geriatrics & Gerontology International.2020; 20(4): 271. CrossRef - Association between sarcopenic obesity and higher risk of type 2 diabetes in adults: A systematic review and meta-analysis
Dima Khadra, Leila Itani, Hana Tannir, Dima Kreidieh, Dana El Masri, Marwan El Ghoch
World Journal of Diabetes.2019; 10(5): 311. CrossRef
- Clinical observation on acupuncture for 80 patients with abdominal obesity in Germany: based on the theory of unblocking and regulating the Belt Vessel
- Epidemiology
- Ten-Year Mortality Trends for Adults with and without Diabetes Mellitus in South Korea, 2003 to 2013
- Kyeong Jin Kim, Tae Yeon Kwon, Sungwook Yu, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Sin Gon Kim, Yousung Park, Nam Hoon Kim
- Diabetes Metab J. 2018;42(5):394-401. Published online April 26, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0088
- 4,862 View
- 58 Download
- 25 Web of Science
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To estimate and compare the trends of all-cause and cause-specific mortality rates for subjects with and without diabetes in South Korea, from 2003 to 2013.
Methods Using a population-based cohort (2003 to 2013), we evaluated annual mortality rates in adults (≥30 years) with and without diabetes. The number of subjects in this analysis ranged from 585,795 in 2003 to 670,020 in 2013.
Results Age- and sex-adjusted all-cause mortality rates decreased consistently in both groups from 2003 to 2013 (from 14.4 to 9.3/1,000 persons in subjects with diabetes and from 7.9 to 4.4/1,000 persons in those without diabetes). The difference in mortality rates between groups also decreased (6.61 per 1,000 persons in 2003 to 4.98 per 1,000 persons in 2013). The slope associated with the mortality rate exhibited a steeper decrease in subjects with diabetes than those without diabetes (regression coefficients of time: −0.50 and −0.33, respectively;
P =0.004). In subjects with diabetes, the mortality rate from cardiovascular disease decreased by 53.5% (from 2.73 to 1.27 per 1,000 persons,P for trend <0.001). Notably, the decrease in mortality from ischemic stroke (79.2%, from 1.20 to 0.25 per 1,000 persowns) was more profound than that from ischemic heart disease (28.3%, from 0.60 to 0.43 per 1,000 persons).Conclusion All-cause and cardiovascular mortality rates decreased substantially from 2003 to 2013, and the decline in ischemic stroke mortality mainly contributed to the decreased cardiovascular mortality in Korean people with diabetes.
-
Citations
Citations to this article as recorded by- Green tea consumption and incidence of cardiovascular disease in type 2 diabetic patients with overweight/obesity: a community-based cohort study
Bingyue Liu, Shujun Gu, Jin Zhang, Hui Zhou, Jian Su, Sudan Wang, Qian Sun, Zhengyuan Zhou, Jinyi Zhou, Chen Dong
Archives of Public Health.2024;[Epub] CrossRef - Trends in all-cause and cause-specific mortality in older adults with and without diabetes: A territory-wide analysis in one million older adults in Hong Kong
Aimin Yang, Tingting Chen, Mai Shi, Eric Lau, Raymond SM Wong, Jones Chan, Juliana CN Chan, Elaine Chow
Diabetes Research and Clinical Practice.2024; 210: 111618. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Letter: Triglyceride-Glucose Index Predicts Cardiovascular Outcome in Metabolically Unhealthy Obese Population: A Nationwide Population-Based Cohort Study (J Obes Metab Syndr 2022;31:178-86)
Gwanpyo Koh
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 179. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - The Characteristics and Risk of Mortality in the Elderly Korean Population
Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 522. CrossRef - Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sung
Diabetes & Metabolism Journal.2022; 46(3): 464. CrossRef - Health-related Quality of Life Instrument With 8 Items for Use in Patients With Type 2 Diabetes Mellitus: A Validation Study in Korea
Juyoung Kim, Hyeon-Jeong Lee, Min-Woo Jo
Journal of Preventive Medicine and Public Health.2022; 55(3): 234. CrossRef - Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
Endocrinology and Metabolism.2022; 37(3): 466. CrossRef - Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
Nam Hoon Kim, Nan Hee Kim
Diabetes & Metabolism Journal.2022; 46(4): 543. CrossRef - Diabetic Ketoacidosis and COVID-19: A Retrospective Observational Study
Govind Nagdev, Gajanan Chavan, Charuta Gadkari, Gaurav Sahu
Cureus.2022;[Epub] CrossRef - Trends in the effects of pre‐transplant diabetes on mortality and cardiovascular events after kidney transplantation
Ja Young Jeon, Soo Jung Kim, Kyoung Hwa Ha, Ji Hyun Park, Bumhee Park, Chang‐Kwon Oh, Seung Jin Han
Journal of Diabetes Investigation.2021; 12(5): 811. CrossRef - Acute Hyperglycemic Crises with Coronavirus Disease-19: Case Reports
Na-young Kim, Eunyeong Ha, Jun Sung Moon, Yong-Hoon Lee, Eun Young Choi
Diabetes & Metabolism Journal.2020; 44(2): 349. CrossRef - Polysomnographic phenotyping of obstructive sleep apnea and its implications in mortality in Korea
Jeong-Whun Kim, Tae-Bin Won, Chae-Seo Rhee, Young Mi Park, In-Young Yoon, Sung-Woo Cho
Scientific Reports.2020;[Epub] CrossRef - Peripheral arterial endothelial dysfunction predicts future cardiovascular events in diabetic patients with albuminuria: a prospective cohort study
Bo Kyung Koo, Woo-Young Chung, Min Kyong Moon
Cardiovascular Diabetology.2020;[Epub] CrossRef - Metformin treatment for patients with diabetes and chronic kidney disease: A Korean Diabetes Association and Korean Society of Nephrology consensus statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Kidney Research and Clinical Practice.2020; 39(1): 32. CrossRef - Outcomes for Inappropriate Renal Dose Adjustment of Dipeptidyl Peptidase-4 Inhibitors in Patients With Type 2 Diabetes Mellitus: Population-Based Study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
Mayo Clinic Proceedings.2020; 95(1): 101. CrossRef - Metformin Treatment for Patients with Diabetes and Chronic Kidney Disease: A Korean Diabetes Association and Korean Society of Nephrology Consensus Statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Diabetes & Metabolism Journal.2020; 44(1): 3. CrossRef - A systematic review of trends in all-cause mortality among people with diabetes
Lei Chen, Rakibul M. Islam, Joanna Wang, Thomas R. Hird, Meda E. Pavkov, Edward W. Gregg, Agus Salim, Maryam Tabesh, Digsu N. Koye, Jessica L. Harding, Julian W. Sacre, Elizabeth L. M. Barr, Dianna J. Magliano, Jonathan E. Shaw
Diabetologia.2020; 63(9): 1718. CrossRef - Diabetic ketoacidosis precipitated by COVID-19: A report of two cases and review of literature
Pavan Kumar Reddy, Mohammad Shafi Kuchay, Yatin Mehta, Sunil Kumar Mishra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(5): 1459. CrossRef - Prognostic value of long-term gamma-glutamyl transferase variability in individuals with diabetes: a nationwide population-based study
Da Young Lee, Kyungdo Han, Ji Hee Yu, Sanghyun Park, Ji A Seo, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Seon Mee Kim, Kyung Mook Choi, Sei Hyun Baik, Yong Gyu Park, Nan Hee Kim
Scientific Reports.2020;[Epub] CrossRef - Arterial stiffness is an independent predictor for risk of mortality in patients with type 2 diabetes mellitus: the REBOUND study
Jeong Mi Kim, Sang Soo Kim, In Joo Kim, Jong Ho Kim, Bo Hyun Kim, Mi Kyung Kim, Soon Hee Lee, Chang Won Lee, Min Chul Kim, Jun Hyeob Ahn, Jinmi Kim
Cardiovascular Diabetology.2020;[Epub] CrossRef - The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMC Medicine.2020;[Epub] CrossRef - Increased Age of Death and Change in Causes of Death Among Persons With Diabetes Mellitus From the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
SSRN Electronic Journal .2020;[Epub] CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Diabetes Mellitus, Still Major Threat to Mortality from Various Causes
Nam Hoon Kim
Diabetes & Metabolism Journal.2019; 43(3): 273. CrossRef - Diabetes and Cancer: Cancer Should Be Screened in Routine Diabetes Assessment
Sunghwan Suh, Kwang-Won Kim
Diabetes & Metabolism Journal.2019; 43(6): 733. CrossRef - Trends of Diabetes Epidemic in Korea
Ji Cheol Bae
Diabetes & Metabolism Journal.2018; 42(5): 377. CrossRef
- Green tea consumption and incidence of cardiovascular disease in type 2 diabetic patients with overweight/obesity: a community-based cohort study
- Clinical Diabetes & Therapeutics
- Changes in the Bone Mineral Density of Femur Neck and Total Hip Over a 52-Week Treatment with Lobeglitazone
- Da Young Lee, Ji A Seo
- Diabetes Metab J. 2017;41(5):374-376. Published online October 24, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.374
- 3,057 View
- 27 Download
- Increased Selenoprotein P Levels in Subjects with Visceral Obesity and Nonalcoholic Fatty Liver Disease
- Hae Yoon Choi, Soon Young Hwang, Chang Hee Lee, Ho Cheol Hong, Sae Jeong Yang, Hye Jin Yoo, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Dong Seop Choi, Kyung Mook Choi
- Diabetes Metab J. 2013;37(1):63-71. Published online February 15, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.1.63
- 4,948 View
- 37 Download
- 85 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Selenoprotein P (SeP) has recently been reported as a novel hepatokine that regulates insulin resistance and systemic energy metabolism in rodents and humans. We explored the associations among SeP, visceral obesity, and nonalcoholic fatty liver disease (NAFLD).
Methods We examined serum SeP concentrations in subjects with increased visceral fat area (VFA) or liver fat accumulation measured with computed tomography. Our study subjects included 120 nondiabetic individuals selected from participants of the Korean Sarcopenic Obesity Study. In addition, we evaluated the relationship between SeP and cardiometabolic risk factors, including homeostasis model of insulin resistance (HOMA-IR), high sensitivity C-reactive protein (hsCRP), adiponectin values, and brachial-ankle pulse wave velocity (baPWV).
Results Subjects with NAFLD showed increased levels of HOMA-IR, hsCRP, VFA, and several components of metabolic syndrome and decreased levels of adiponectin and high density lipoprotein cholesterol than those of controls. Serum SeP levels were positively correlated with VFA, hsCRP, and baPWV and negatively correlated with the liver attenuation index. Not only subjects with visceral obesity but also those with NAFLD exhibited significantly increased SeP levels (
P <0.001). In multiple logistic regression analysis, the subjects in the highest SeP tertile showed a higher risk for NAFLD than those in the lowest SeP tertile, even after adjusting for potential confounding factors (odds ratio, 7.48; 95% confidence interval, 1.72 to 32.60;P =0.007).Conclusion Circulating SeP levels were increased in subjects with NAFLD as well as in those with visceral obesity and may be a novel biomarker for NAFLD.
-
Citations
Citations to this article as recorded by- Myosteatosis: Diagnosis, pathophysiology and consequences in metabolic dysfunction-associated steatotic liver disease
Guillaume Henin, Audrey Loumaye, Isabelle A. Leclercq, Nicolas Lanthier
JHEP Reports.2024; 6(2): 100963. CrossRef - Association between serum trace element, mineral, and amino acid levels with non-alcoholic fatty liver disease (NAFLD) in adult women
Alexey A. Tinkov, Tatiana V. Korobeinikova, Galina D. Morozova, Michael Aschner, Daria V. Mak, Abel Santamaria, Joao B.T. Rocha, Tatiana I. Sotnikova, Serafima Ia. Tazina, Anatoly V. Skalny
Journal of Trace Elements in Medicine and Biology.2024; 83: 127397. CrossRef - Adipose-derived extracellular vesicles – a novel cross-talk mechanism in insulin resistance, non-alcoholic fatty liver disease, and polycystic ovary syndrome
Dušan Mladenović, Milena Vesković, Nikola Šutulović, Dragan Hrnčić, Olivera Stanojlović, Lena Radić, Jelica Bjekić Macut, Djuro Macut
Endocrine.2024;[Epub] CrossRef - Association of metabolic-dysfunction associated steatotic liver disease with polycystic ovary syndrome
Qiuyu Xu, Jie Zhang, Yan Lu, Ling Wu
iScience.2024; 27(2): 108783. CrossRef - The role of hepatokines in NAFLD
Norbert Stefan, Fritz Schick, Andreas L. Birkenfeld, Hans-Ulrich Häring, Morris F. White
Cell Metabolism.2023; 35(2): 236. CrossRef - The regulatory role of metabolic organ-secreted factors in the nonalcoholic fatty liver disease and cardiovascular disease
Li Qin, Junru Wu, Xuejing Sun, Xuewei Huang, Wei Huang, Chunyan Weng, Jingjing Cai
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - The Role of Organokines in Obesity and Type 2 Diabetes and Their Functions as Molecular Transducers of Nutrition and Exercise
Ji Ye Lim, Eunju Kim
Metabolites.2023; 13(9): 979. CrossRef - Hepatokine Profile in Adolescents with Polycystic Ovary Syndrome: A Case–Control Study
Aikaterini Giannouli, Charikleia Stefanaki, Christos Kouskoutis, Marianna Konidari, Iliana Mani, Konstantina Konidari, Sophia L. Markantonis, Aimilia Mantzou, Spyridon P. Dourakis, Efthymios Deligeoroglou, Flora Bacopoulou
Journal of Clinical Medicine.2023; 12(17): 5744. CrossRef - The Interconnection between Hepatic Insulin Resistance and Metabolic Dysfunction-Associated Steatotic Liver Disease—The Transition from an Adipocentric to Liver-Centric Approach
Milena Vesković, Nikola Šutulović, Dragan Hrnčić, Olivera Stanojlović, Djuro Macut, Dušan Mladenović
Current Issues in Molecular Biology.2023; 45(11): 9084. CrossRef - Sulforaphane decreases serum selenoprotein P levels through enhancement of lysosomal degradation independent of Nrf2
Xinying Ye, Takashi Toyama, Keiko Taguchi, Kotoko Arisawa, Takayuki Kaneko, Ryouhei Tsutsumi, Masayuki Yamamoto, Yoshiro Saito
Communications Biology.2023;[Epub] CrossRef - “Alphabet” Selenoproteins: Implications in Pathology
Carmen Beatrice Dogaru, Carmen Duță, Corina Muscurel, Irina Stoian
International Journal of Molecular Sciences.2023; 24(20): 15344. CrossRef - Metabolic dysfunction-associated steatotic liver disease and the heart
Stan Driessen, Sven M. Francque, Stefan D. Anker, Manuel Castro Cabezas, Diederick E. Grobbee, Maarten E. Tushuizen, Adriaan G. Holleboom
Hepatology.2023;[Epub] CrossRef - Associations between Circulating SELENOP Level and Disorders of Glucose and Lipid Metabolism: A Meta-Analysis
Ruirui Yu, Zhoutian Wang, Miaomiao Ma, Ping Xu, Longjian Liu, Alexey A. Tinkov, Xin Gen Lei, Ji-Chang Zhou
Antioxidants.2022; 11(7): 1263. CrossRef - Contribution of organokines in the development of NAFLD/NASH associated hepatocellular carcinoma
Meenakshi Vachher, Savita Bansal, Bhupender Kumar, Sandeep Yadav, Taruna Arora, Nalini Moza Wali, Archana Burman
Journal of Cellular Biochemistry.2022; 123(10): 1553. CrossRef - Regulatory network and interplay of hepatokines, stellakines, myokines and adipokines in nonalcoholic fatty liver diseases and nonalcoholic steatohepatitis
Bing Yang, Liqing Lu, Dongmei Zhou, Wei Fan, Lucía Barbier-Torres, Justin Steggerda, Heping Yang, Xi Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Cytokines and regulation of glucose and lipid metabolism in the obesity
V. I. Scherbakov, G. A. Skosyreva, T. I. Ryabichenko, O. O. Obukhova
Obesity and metabolism.2022; 19(3): 317. CrossRef - SeP is elevated in NAFLD and participates in NAFLD pathogenesis through AMPK/ACC pathway
Yi Chen, Xinjue He, Xueyang Chen, Youming Li, Yini Ke
Journal of Cellular Physiology.2021; 236(5): 3800. CrossRef - Hepatokines and metabolism: Deciphering communication from the liver
Sharon O. Jensen-Cody, Matthew J. Potthoff
Molecular Metabolism.2021; 44: 101138. CrossRef - Weight-loss-independent benefits of exercise on liver steatosis and stiffness in Japanese men with NAFLD
Sechang Oh, Takehiko Tsujimoto, Bokun Kim, Fumihiko Uchida, Hideo Suzuki, Seiichiro Iizumi, Tomonori Isobe, Takeji Sakae, Kiyoji Tanaka, Junichi Shoda
JHEP Reports.2021; 3(3): 100253. CrossRef - Efficacy of Weight Reduction on Pediatric Nonalcoholic Fatty Liver Disease: Opportunities to Improve Treatment Outcomes Through Pharmacotherapy
Chance S. Friesen, Chelsea Hosey-Cojocari, Sherwin S. Chan, Iván L. Csanaky, Jonathan B. Wagner, Brooke R. Sweeney, Alec Friesen, Jason D. Fraser, Valentina Shakhnovich
Frontiers in Endocrinology.2021;[Epub] CrossRef - Association of Urinary and Dietary Selenium and of Serum Selenium Species with Serum Alanine Aminotransferase in a Healthy Italian Population
Teresa Urbano, Tommaso Filippini, Daniela Lasagni, Tiziana De Luca, Peter Grill, Sabrina Sucato, Elisa Polledri, Guy Djeukeu Noumbi, Marcella Malavolti, Annalisa Santachiara, Thelma A. Pertinhez, Roberto Baricchi, Silvia Fustinoni, Bernhard Michalke, Marc
Antioxidants.2021; 10(10): 1516. CrossRef - Selenotranscriptome Network in Non-alcoholic Fatty Liver Disease
Kaitlin Day, Lucia A. Seale, Ross M. Graham, Barbara R. Cardoso
Frontiers in Nutrition.2021;[Epub] CrossRef - Hepatokines and Non-Alcoholic Fatty Liver Disease: Linking Liver Pathophysiology to Metabolism
Tae Hyun Kim, Dong-Gyun Hong, Yoon Mee Yang
Biomedicines.2021; 9(12): 1903. CrossRef - Leukocyte cell-derived chemotaxin-2 and fibroblast growth factor 21 in alcohol-induced liver cirrhosis
Jarosław Jerzy Sak, Andrzej Prystupa, Paweł Kiciński, Dorota Luchowska-Kocot, Ewa Kurys-Denis, Hanna Bis-Wencel
World Journal of Hepatology.2021; 13(12): 2071. CrossRef - Acute Hyperenergetic, High-Fat Feeding Increases Circulating FGF21, LECT2, and Fetuin-A in Healthy Men
Scott A Willis, Jack A Sargeant, Thomas Yates, Toshinari Takamura, Hiroaki Takayama, Vinay Gupta, Emily Brittain, Joe Crawford, Siôn A Parry, Alice E Thackray, Veronica Varela-Mato, David J Stensel, Rachel M Woods, Carl J Hulston, Guruprasad P Aithal, Jam
The Journal of Nutrition.2020; 150(5): 1076. CrossRef - Targeting fibrinogen‐like protein 1 is a novel therapeutic strategy to combat obesity
Hung‐Tsung Wu, Szu‐Chi Chen, Kang‐Chih Fan, Chun‐Heng Kuo, Shin‐Yu Lin, Shu‐Huei Wang, Chih‐Jen Chang, Hung‐Yuan Li
The FASEB Journal.2020; 34(2): 2958. CrossRef - Nonalcoholic fatty liver disease and cardiovascular disease phenotypes
Giandomenico Bisaccia, Fabrizio Ricci, Cesare Mantini, Claudio Tana, Gian Luca Romani, Cosima Schiavone, Sabina Gallina
SAGE Open Medicine.2020; 8: 205031212093380. CrossRef - Higher Serum Selenoprotein P Level as a Novel Inductor of Metabolic Complications in Psoriasis
Anna Baran, Julia Nowowiejska, Julita Anna Krahel, Tomasz W. Kaminski, Magdalena Maciaszek, Iwona Flisiak
International Journal of Molecular Sciences.2020; 21(13): 4594. CrossRef - The Role of Exercise in the Interplay between Myokines, Hepatokines, Osteokines, Adipokines, and Modulation of Inflammation for Energy Substrate Redistribution and Fat Mass Loss: A Review
Adrian M. Gonzalez-Gil, Leticia Elizondo-Montemayor
Nutrients.2020; 12(6): 1899. CrossRef - Selenoprotein P; P for Plasma, Prognosis, Prophylaxis, and More
Ryouhei Tsutsumi, Yoshiro Saito
Biological and Pharmaceutical Bulletin.2020; 43(3): 366. CrossRef - Selenium and selenoprotein P in nonalcoholic fatty liver disease
Stergios A. Polyzos, Jannis Kountouras, Antonis Goulas, Leonidas Duntas
Hormones.2020; 19(1): 61. CrossRef - The Effects of Endoplasmic-Reticulum-Resident Selenoproteins in a Nonalcoholic Fatty Liver Disease Pig Model Induced by a High-Fat Diet
Pengzu Wang, Zhuang Lu, Meng He, Baoming Shi, Xingen Lei, Anshan Shan
Nutrients.2020; 12(3): 692. CrossRef - The risk of pregnancy‐associated hypertension in women with nonalcoholic fatty liver disease
Young Mi Jung, Seung Mi Lee, Subeen Hong, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan‐Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Liver International.2020; 40(10): 2417. CrossRef - Why Multiples of 21? Why does Selenoprotein P Contain Multiple Selenocysteine Residues?
Janinah Baclaocos, John James Mackrill
Current Nutraceuticals.2020; 1(1): 42. CrossRef - Selenium and Selenoproteins in Adipose Tissue Physiology and Obesity
Alexey A. Tinkov, Olga P. Ajsuvakova, Tommaso Filippini, Ji-Chang Zhou, Xin Gen Lei, Eugenia R. Gatiatulina, Bernhard Michalke, Margarita G. Skalnaya, Marco Vinceti, Michael Aschner, Anatoly V. Skalny
Biomolecules.2020; 10(4): 658. CrossRef - Metabolic adaptations after bariatric surgery: adipokines, myokines and hepatokines
Justine Faramia, Giada Ostinelli, Virginie Drolet-Labelle, Frédéric Picard, André Tchernof
Current Opinion in Pharmacology.2020; 52: 67. CrossRef - Physiopathology of Lifestyle Interventions in Non-Alcoholic Fatty Liver Disease (NAFLD)
David Carneros, Guillermo López-Lluch, Matilde Bustos
Nutrients.2020; 12(11): 3472. CrossRef - Interplay between Oxidative Stress and Metabolic Derangements in Non-Alcoholic Fatty Liver Disease: The Role of Selenoprotein P
Gian Paolo Caviglia, Chiara Rosso, Angelo Armandi, Melania Gaggini, Fabrizia Carli, Maria Lorena Abate, Antonella Olivero, Davide Giuseppe Ribaldone, Giorgio Maria Saracco, Amalia Gastaldelli, Elisabetta Bugianesi
International Journal of Molecular Sciences.2020; 21(22): 8838. CrossRef - Can hepatokines be regarded as novel non-invasive serum biomarkers of intrahepatic lipid content in obese children?
Marta Flisiak-Jackiewicz, Anna Bobrus-Chociej, Natalia Wasilewska, Eugeniusz Tarasow, Malgorzata Wojtkowska, Dariusz Marek Lebensztejn
Advances in Medical Sciences.2019; 64(2): 280. CrossRef - Dietary pattern associated with selenoprotein P and MRI-derived body fat volumes, liver signal intensity, and metabolic disorders
Romina di Giuseppe, Sandra Plachta-Danielzik, Manja Koch, Ute Nöthlings, Sabrina Schlesinger, Jan Borggrefe, Marcus Both, Hans-Peter Müller, Jan Kassubek, Gunnar Jacobs, Wolfgang Lieb
European Journal of Nutrition.2019; 58(3): 1067. CrossRef - Cytokines and Abnormal Glucose and Lipid Metabolism
Jie Shi, Jiangao Fan, Qing Su, Zhen Yang
Frontiers in Endocrinology.2019;[Epub] CrossRef - Role of exercise-induced hepatokines in metabolic disorders
Gaël Ennequin, Pascal Sirvent, Martin Whitham
American Journal of Physiology-Endocrinology and Metabolism.2019; 317(1): E11. CrossRef - Metabolomics signature associated with circulating serum selenoprotein P levels
Romina di Giuseppe, Manja Koch, Ute Nöthlings, Gabi Kastenmüller, Anna Artati, Jerzy Adamski, Gunnar Jacobs, Wolfgang Lieb
Endocrine.2019; 64(3): 486. CrossRef - Secretomics to Discover Regulators in Diseases
Parkyong Song, Yonghoon Kwon, Jae-Yeol Joo, Do-Geun Kim, Jong Hyuk Yoon
International Journal of Molecular Sciences.2019; 20(16): 3893. CrossRef - Impact of Lipotoxicity on Tissue “Cross Talk” and Metabolic Regulation
Magdalene K. Montgomery, William De Nardo, Matthew J. Watt
Physiology.2019; 34(2): 134. CrossRef - The Liver as an Endocrine Organ—Linking NAFLD and Insulin Resistance
Matthew J Watt, Paula M Miotto, William De Nardo, Magdalene K Montgomery
Endocrine Reviews.2019; 40(5): 1367. CrossRef - Inter-organ cross-talk in metabolic syndrome
Christina Priest, Peter Tontonoz
Nature Metabolism.2019; 1(12): 1177. CrossRef - Serum selenoprotein P, but not selenium, predicts future hyperglycemia in a general Japanese population
Swe Mar Oo, Hirofumi Misu, Yoshiro Saito, Mutsumi Tanaka, Seiji Kato, Yuki Kita, Hiroaki Takayama, Yumie Takeshita, Takehiro Kanamori, Toru Nagano, Masatoshi Nakagen, Takeshi Urabe, Naoto Matsuyama, Shuichi Kaneko, Toshinari Takamura
Scientific Reports.2018;[Epub] CrossRef - NAFLD and cardiovascular disease
Elisabete Martins, Ana Oliveira
Porto Biomedical Journal.2018; 3(2): e2. CrossRef - The influence of adiposity and acute exercise on circulating hepatokines in normal-weight and overweight/obese men
Jack A. Sargeant, Guruprasad P. Aithal, Toshinari Takamura, Hirofumi Misu, Hiroaki Takayama, Jessica A. Douglas, Mark C. Turner, David J. Stensel, Myra A. Nimmo, David R. Webb, Thomas Yates, James A. King
Applied Physiology, Nutrition, and Metabolism.2018; 43(5): 482. CrossRef - Low Urine pH Is Associated with Non-alcoholic Fatty Liver Disease: A Community-based Cross-sectional Study
Teruki Miyake, Sakiko Yoshida, Shin Yamamoto, Shinya Furukawa, Osamu Yoshida, Sayaka Kanzaki, Hidenori Senba, Toru Ishihara, Mitsuhito Koizumi, Yoshio Tokumoto, Masashi Hirooka, Teru Kumagi, Masanori Abe, Kohichiro Kitai, Bunzo Matsuura, Yoichi Hiasa
Internal Medicine.2018; 57(19): 2799. CrossRef - Evaluation of endothelial dysfunction in patients with nonalcoholic fatty liver disease: Association of selenoprotein P with carotid intima-media thickness and endothelium-dependent vasodilation
Ibrahim Cetindağlı, Muammer Kara, Alpaslan Tanoglu, Veysel Ozalper, Serkan Aribal, Yusuf Hancerli, Mehmet Unal, Onur Ozarı, Serdar Hira, Mustafa Kaplan, Yusuf Yazgan
Clinics and Research in Hepatology and Gastroenterology.2017; 41(5): 516. CrossRef - Differences in the risk of fatty liver for onset of impaired fasting glucose according to baseline plasma glucose levels
Teruki Miyake, Masashi Hirooka, Osamu Yoshida, Shinya Furukawa, Teru Kumagi, Mitsuhito Koizumi, Shin Yamamoto, Taira Kuroda, Eiji Arimitsu, Eiji Takeshita, Masanori Abe, Kohichiro Kitai, Bunzo Matsuura, Yoichi Hiasa
Journal of Gastroenterology.2017; 52(2): 237. CrossRef - Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance
Ruth C. R. Meex, Matthew J. Watt
Nature Reviews Endocrinology.2017; 13(9): 509. CrossRef - Circulating selenoprotein P levels in relation to MRI‐derived body fat volumes, liver fat content, and metabolic disorders
Romina di Giuseppe, Manja Koch, Sabrina Schlesinger, Jan Borggrefe, Marcus Both, Hans‐Peter Müller, Jan Kassubek, Gunnar Jacobs, Ute Nöthlings, Wolfgang Lieb
Obesity.2017; 25(6): 1128. CrossRef - Eicosapentaenoic acid down-regulates expression of the selenoprotein P gene by inhibiting SREBP-1c protein independently of the AMP-activated protein kinase pathway in H4IIEC3 hepatocytes
Natsumi Tajima-Shirasaki, Kiyo-aki Ishii, Hiroaki Takayama, Takayoshi Shirasaki, Hisakazu Iwama, Keita Chikamoto, Yoshiro Saito, Yasumasa Iwasaki, Atsushi Teraguchi, Fei Lan, Akihiro Kikuchi, Yumie Takeshita, Koji Murao, Seiichi Matsugo, Shuichi Kaneko, H
Journal of Biological Chemistry.2017; 292(26): 10791. CrossRef - Selenoprotein P is elevated in individuals with obesity, but is not independently associated with insulin resistance
Miaoxin Chen, Bo Liu, David Wilkinson, Amy T. Hutchison, Campbell H. Thompson, Gary A. Wittert, Leonie K. Heilbronn
Obesity Research & Clinical Practice.2017; 11(2): 227. CrossRef - Cardiovascular Risk in Patients with Non-alcoholic Fatty Liver Disease
Hak Soo Kim, Yong Kyun Cho
The Korean Journal of Gastroenterology.2017; 69(6): 333. CrossRef - Association between betatrophin/ANGPTL8 and non-alcoholic fatty liver disease: animal and human studies
Yong-ho Lee, Sang-Guk Lee, Chan Joo Lee, Soo Hyun Kim, Young-Mi Song, Mi Ra Yoon, Byung Hun Jeon, Jae Hyuk Lee, Byung-Wan Lee, Eun Seok Kang, Hyun Chul Lee, Bong-Soo Cha
Scientific Reports.2016;[Epub] CrossRef - Implication of hepatokines in metabolic disorders and cardiovascular diseases
Tae Woo Jung, Hye Jin Yoo, Kyung Mook Choi
BBA Clinical.2016; 5: 108. CrossRef - Selenoproteins: Antioxidant selenoenzymes and beyond
Holger Steinbrenner, Bodo Speckmann, Lars-Oliver Klotz
Archives of Biochemistry and Biophysics.2016; 595: 113. CrossRef - Metabolic Adaptation in Obesity and Type II Diabetes: Myokines, Adipokines and Hepatokines
Kyoung-Jin Oh, Da Lee, Won Kim, Baek Han, Sang Lee, Kwang-Hee Bae
International Journal of Molecular Sciences.2016; 18(1): 8. CrossRef - Pathogenesis of nonalcoholic steatohepatitis
Wensheng Liu, Robert D. Baker, Tavleen Bhatia, Lixin Zhu, Susan S. Baker
Cellular and Molecular Life Sciences.2016; 73(10): 1969. CrossRef - Stéatose et résistance à l’insuline : implication des hépatokines
C. Bertrand, P. Valet, I. Castan-Laurell
Obésité.2016; 11(3): 170. CrossRef - Pathophysiology of Non Alcoholic Fatty Liver Disease
Salvatore Petta, Amalia Gastaldelli, Eleni Rebelos, Elisabetta Bugianesi, Piergiorgio Messa, Luca Miele, Gianluca Svegliati-Baroni, Luca Valenti, Ferruccio Bonino
International Journal of Molecular Sciences.2016; 17(12): 2082. CrossRef - Alterations in serum levels of fetuin A and selenoprotein P in chronic hepatitis C patients with concomitant type 2 diabetes: A case-control study
Sahar A. Ali, Walaa M.H. Nassif, Dalia H.A. Abdelaziz
Clinics and Research in Hepatology and Gastroenterology.2016; 40(4): 465. CrossRef - Non-alcoholic fatty liver disease and cardiovascular risk: Pathophysiological mechanisms and implications
Sven M. Francque, Denise van der Graaff, Wilhelmus J. Kwanten
Journal of Hepatology.2016; 65(2): 425. CrossRef - “Omics” of Selenium Biology: A Prospective Study of Plasma Proteome Network Before and After Selenized-Yeast Supplementation in Healthy Men
Indu Sinha, Kubra Karagoz, Rachel L. Fogle, Christopher S. Hollenbeak, Arnold H. Zea, Kazim Y. Arga, Anne E. Stanley, Wayne C. Hawkes, Raghu Sinha
OMICS: A Journal of Integrative Biology.2016; 20(4): 202. CrossRef - Nonalcoholic steatohepatitis is strongly associated with sarcopenic obesity in patients with cirrhosis undergoing liver transplant evaluation
Sandra Carias, Ana Lia Castellanos, Valery Vilchez, Rashmi Nair, Anna Christina Dela Cruz, Jennifer Watkins, Terrence Barrett, Patel Trushar, Karyn Esser, Roberto Gedaly
Journal of Gastroenterology and Hepatology.2016; 31(3): 628. CrossRef - Variants in Genes Controlling Oxidative Metabolism Contribute to Lower Hepatic ATP Independent of Liver Fat Content in Type 1 Diabetes
Sofiya Gancheva, Alessandra Bierwagen, Kirti Kaul, Christian Herder, Peter Nowotny, Sabine Kahl, Guido Giani, Birgit Klueppelholz, Birgit Knebel, Paul Begovatz, Klaus Strassburger, Hadi Al-Hasani, Jesper Lundbom, Julia Szendroedi, Michael Roden
Diabetes.2016; 65(7): 1849. CrossRef - Selenoprotein P is not elevated in gestational diabetes mellitus
Alev E. Altinova, Ozlem T. Iyidir, Cigdem Ozkan, Damla Ors, Merve Ozturk, Ozlem Gulbahar, Nuray Bozkurt, Fusun B. Toruner, Mujde Akturk, Nuri Cakir, Metin Arslan
Gynecological Endocrinology.2015; 31(11): 874. CrossRef - Selenium and Human Health: Witnessing a Copernican Revolution?
Ewa Jablonska, Marco Vinceti
Journal of Environmental Science and Health, Part C.2015; 33(3): 328. CrossRef - Toenail selenium and risk of type 2 diabetes: the ORDET cohort study
Marco Vinceti, Sara Grioni, Dorothea Alber, Dario Consonni, Carlotta Malagoli, Claudia Agnoli, Marcella Malavolti, Valeria Pala, Vittorio Krogh, Sabina Sieri
Journal of Trace Elements in Medicine and Biology.2015; 29: 145. CrossRef - Expression of Selenoprotein Genes Is Affected by Obesity of Pigs Fed a High-Fat Diet
Hua Zhao, Ke Li, Jia-Yong Tang, Ji-Chang Zhou, Kang-Ning Wang, Xin-Jie Xia, Xin Gen Lei
The Journal of Nutrition.2015; 145(7): 1394. CrossRef - Hepatokines as a Link between Obesity and Cardiovascular Diseases
Hye Jin Yoo, Kyung Mook Choi
Diabetes & Metabolism Journal.2015; 39(1): 10. CrossRef - The Dipeptidyl Peptidase-4 Inhibitor Teneligliptin Attenuates Hepatic Lipogenesis via AMPK Activation in Non-Alcoholic Fatty Liver Disease Model Mice
Takayasu Ideta, Yohei Shirakami, Tsuneyuki Miyazaki, Takahiro Kochi, Hiroyasu Sakai, Hisataka Moriwaki, Masahito Shimizu
International Journal of Molecular Sciences.2015; 16(12): 29207. CrossRef - Dietary selenate attenuates adiposity and improves insulin sensitivity in high-fat diet-induced obese mice
Choon Young Kim, Yuyan Zhu, Kimberly K. Buhman, Kee-Hong Kim
Journal of Functional Foods.2015; 17: 33. CrossRef - Use of a Diabetes Self-Assessment Score to Predict Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis
Gyuri Kim, Yong-ho Lee, Young Min Park, Jungghi Kim, Heesuk Kim, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Dae Jung Kim
Medicine.2015; 94(27): e1103. CrossRef - Inhibition of SH2-domain-containing inositol 5-phosphatase (SHIP2) ameliorates palmitate induced-apoptosis through regulating Akt/FOXO1 pathway and ROS production in HepG2 cells
Sattar Gorgani-Firuzjaee, Khosrow Adeli, Reza Meshkani
Biochemical and Biophysical Research Communications.2015; 464(2): 441. CrossRef - Exendin-4 Inhibits the Expression of SEPP1 and Fetuin-A via Improvement of Palmitic Acid-Induced Endoplasmic Reticulum Stress by AMPK
Jinmi Lee, Seok-Woo Hong, Se Eun Park, Eun-Jung Rhee, Cheol-Young Park, Ki-Won Oh, Sung-Woo Park, Won-Young Lee
Endocrinology and Metabolism.2015; 30(2): 177. CrossRef - AMPK activator-mediated inhibition of endoplasmic reticulum stress ameliorates carrageenan-induced insulin resistance through the suppression of selenoprotein P in HepG2 hepatocytes
Tae Woo Jung, So Young Lee, Ho Cheol Hong, Hae Yoon Choi, Hye Jin Yoo, Sei Hyun Baik, Kyung Mook Choi
Molecular and Cellular Endocrinology.2014; 382(1): 66. CrossRef - HIF‐1α Expression as a Protective Strategy of HepG2 Cells Against Fatty Acid‐Induced Toxicity
Wonbaek Yoo, Kyung Hee Noh, Jae Hee Ahn, Ji Hee Yu, Ji A. Seo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Tae Woo Kim, Hyo Joon Kim, Nan Hee Kim
Journal of Cellular Biochemistry.2014; 115(6): 1147. CrossRef - Genetic variants in selenoprotein P plasma 1 gene (SEPP1) are associated with fasting insulin and first phase insulin response in Hispanics
Jacklyn N. Hellwege, Nicholette D. Palmer, Julie T. Ziegler, Carl D. Langefeld, Carlos Lorenzo, Jill M. Norris, Toshinari Takamura, Donald W. Bowden
Gene.2014; 534(1): 33. CrossRef - Levels of circulating selenoprotein P, fibroblast growth factor (FGF) 21 and FGF23 in relation to the metabolic syndrome in young children
B-J Ko, S M Kim, K H Park, H S Park, C S Mantzoros
International Journal of Obesity.2014; 38(12): 1497. CrossRef - The association between non-alcoholic fatty liver disease and carotid atherosclerosis in subjects with within-reference range alanine aminotransferase levels
Kyung-Soo Kim, Hyun-Ju Oh, Dae-Jung Kim, Soo-Kyung Kim, Seok Won Park, Yong-Wook Cho, Kap-Bum Huh
Endocrine Journal.2013; 60(12): 1295. CrossRef
- Myosteatosis: Diagnosis, pathophysiology and consequences in metabolic dysfunction-associated steatotic liver disease

 KDA
KDA
 First
First Prev
Prev





